Get Tb Test Form in PDF
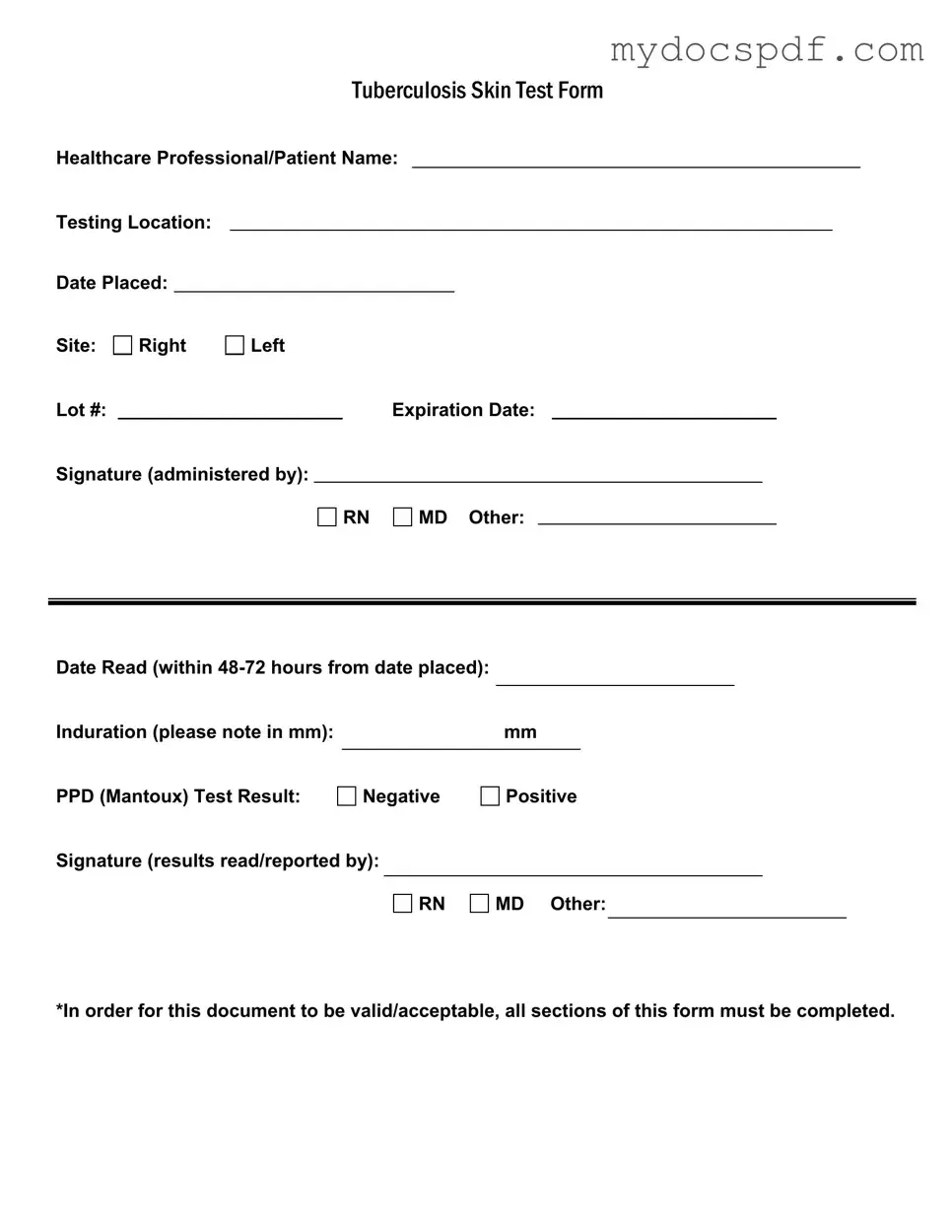
When it comes to assessing exposure to tuberculosis, the Tb Test form plays a crucial role in ensuring accurate and reliable results. This essential document captures vital information about the healthcare professional administering the test, as well as the patient being tested. Key details such as the testing location, the date the test was placed, and the site of administration—whether on the right or left arm—are all recorded meticulously. The form also includes specific identifiers like the lot number and expiration date of the testing material, which are important for maintaining the integrity of the test. After the test is administered, it is imperative to read the results within 48 to 72 hours, and this timeframe is noted on the form. The induration, measured in millimeters, provides a quantitative assessment of the test outcome, which can be either negative or positive. To validate the results, signatures from the administering professional and the individual reading the results are required, ensuring accountability at each step. Completing all sections of this form is not just a formality; it is essential for the document to be considered valid and acceptable in medical and legal contexts.
Dos and Don'ts
When filling out the Tuberculosis (TB) Test form, it's important to ensure accuracy and completeness. Here are some guidelines to follow:
- Do fill in all required fields completely. This includes your name, testing location, and the date the test was placed.
- Do double-check the expiration date of the test materials to ensure they are still valid.
- Do make sure to indicate the site of the test clearly, whether it’s the right or left arm.
- Do sign the form where required to validate the administration and reading of the test.
- Don't leave any sections blank, as this could invalidate the form.
- Don't forget to note the induration measurement in millimeters accurately.
- Don't use abbreviations or unclear language; clarity is key for accurate reporting.
- Don't overlook the importance of timely reading of the test results, which should occur within 48-72 hours.
Document Attributes
| Fact Name | Description |
|---|---|
| Form Title | The form is officially titled "Tuberculosis Skin Test Form." It is used to document the administration and results of the TB skin test. |
| Healthcare Professional | The form requires the name of the healthcare professional administering the test, such as an RN or MD. |
| Testing Location | It is essential to include the location where the test is administered, ensuring proper record-keeping. |
| Date Placed | The date the test is administered must be recorded for accurate tracking of results. |
| Site of Administration | The form specifies whether the test is placed on the right or left arm, which is important for evaluation. |
| Lot Number | The lot number of the PPD solution used must be noted to ensure traceability and safety. |
| Expiration Date | It is crucial to record the expiration date of the PPD solution to avoid using expired materials. |
| Date Read | The results must be read within 48 to 72 hours after placement, and this date must be documented. |
| Induration Measurement | The induration, measured in millimeters, indicates the reaction to the test and must be accurately noted. |
| Test Result | The form requires a clear indication of whether the test result is negative or positive, which is critical for patient care. |
Key takeaways
When filling out the TB Test form, keep these key points in mind:
- Complete all sections: Ensure every part of the form is filled out. Missing information can make the document invalid.
- Provide accurate dates: Record the date the test is placed and the date it is read. The reading must occur within 48-72 hours.
- Indicate the site: Clearly mark whether the test was placed on the right or left arm.
- Note the induration: Measure and record the induration in millimeters. This is crucial for determining the test result.
- Signature requirements: Ensure the form is signed by the healthcare professional who administered the test and the one who read the results.
- Check expiration dates: Make sure the lot number and expiration date are noted, as these affect the validity of the test.
Other PDF Templates
Fedex Indirect Signature - Tracking information can be accessed at fedex.com for your convenience.
Irs Streamlined Filing Compliance Procedures - Form 14653 aims to assist in correcting past filing issues without severe penalties.
In addition to the importance of the Texas Motor Vehicle Bill of Sale form, obtaining a comprehensive template can greatly assist in the completion process. You can find a useful resource at Texas Forms Online, which can provide guidance and ensure that all necessary information is captured correctly for the transaction.
Blank Ada Claim Form - Authorize payment of dental benefits to the provider.
Example - Tb Test Form
|
|
|
|
|
TUBERCULOSISSKINTESTFORM |
||||||||
Healthcare Professional/Patient Name: |
|||||||||||||
Testing Location: |
|
|
|
|
|
|
|
|
|
|
|
||
Date Placed: |
|
|
|
|
|
|
|
|
|
|
|
|
|
Site: |
Right |
Left |
|
|
|
|
|
|
|
|
|||
Lot #: |
|
|
|
|
|
Expiration Date: |
|
|
|||||
Signature (administered by): |
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
RN |
|
MD Other: |
|
|
|
|||
Date Read (within |
|
|
|
|
|
|
|
Induration (please note in mm): |
|
mm |
|
PPD (Mantoux) Test Result: |
|
|
|
Negative |
Positive |
||
Signature (results read/reported by):
RN
MD Other:
*In order for this document to be valid/acceptable, all sections of this form must be completed.
Detailed Instructions for Writing Tb Test
After obtaining the Tb Test form, it is important to fill it out accurately to ensure it is valid and acceptable. Each section of the form requires specific information, which must be completed to avoid any issues.
- Begin by entering the Healthcare Professional/Patient Name at the top of the form.
- Next, fill in the Testing Location where the test is being administered.
- Record the Date Placed on the form, which is the date the test is conducted.
- Indicate the Site of the test by checking either the Right or Left option.
- Enter the Lot # of the test used for the administration.
- Provide the Expiration Date of the test.
- Have the administering professional sign the form, selecting their title: RN, MD, or Other.
- Fill in the Date Read, which must be within 48-72 hours from the Date Placed.
- Measure and note the Induration in millimeters (mm) on the form.
- Mark the PPD (Mantoux) Test Result as either Negative or Positive.
- Finally, have the professional who reads the results sign the form, again selecting their title: RN, MD, or Other.
Documents used along the form
The Tuberculosis (TB) Test form is a crucial document used in healthcare settings to record the administration and results of a TB skin test. However, several other forms and documents are often used in conjunction with the TB Test form to ensure comprehensive patient care and accurate record-keeping. Below is a list of these documents, each serving a specific purpose in the healthcare process.
- Patient Medical History Form: This form gathers essential information about the patient's past medical conditions, medications, and allergies. It helps healthcare providers understand the patient's overall health and any potential risks associated with the TB test.
- Informed Consent Form: Before administering the TB test, patients must provide consent. This form ensures that patients are fully informed about the procedure, its purpose, and any potential risks involved.
- TB Screening Questionnaire: This document includes a series of questions designed to identify risk factors for tuberculosis. It helps healthcare providers assess whether a patient is at higher risk and may require additional testing or monitoring.
- Referral Form: If a patient tests positive for TB, a referral form may be necessary to direct them to a specialist for further evaluation and treatment. This ensures that patients receive appropriate care promptly.
- Follow-Up Appointment Schedule: After the TB test, a follow-up appointment may be necessary to discuss results and next steps. This schedule helps keep both the patient and healthcare provider organized and informed.
- Dog Bill of Sale: For transferring canine ownership, the comprehensive Dog Bill of Sale form guide is essential to ensure a smooth transaction.
- Immunization Record: This document tracks a patient's vaccination history. It may be relevant in assessing overall health and determining if additional immunizations are needed, particularly in relation to TB prevention.
- Laboratory Results Form: If additional tests are required, such as a chest X-ray or blood test, this form records the results. It is vital for making informed decisions about the patient's health and treatment options.
- Patient Education Materials: These materials provide information about tuberculosis, its transmission, and prevention strategies. They are essential for empowering patients to take an active role in their health.
- Insurance Information Form: This document collects details about the patient's insurance coverage. It ensures that the costs associated with the TB test and any follow-up care are appropriately managed.
In summary, while the TB Test form is an essential component of tuberculosis screening, it is accompanied by several other documents that facilitate patient care and ensure that all necessary information is collected and shared. Each of these forms plays a vital role in the overall healthcare process, helping to provide comprehensive support to patients undergoing TB testing and treatment.