Get Progress Notes Form in PDF
The Progress Notes form serves as a crucial component in the documentation of patient care within medical facilities. Designed to capture essential information, this standardized form includes sections for the patient's identification, such as their name, grade, rank, and hospital or medical facility details. Each entry is dated, ensuring a clear timeline of the patient's medical history and treatment. The form adheres to the guidelines set forth by the General Services Administration and the Federal Information Resources Management Regulation, reflecting the importance of consistent record-keeping in healthcare. By utilizing the Progress Notes form, healthcare professionals can effectively communicate changes in a patient's condition, treatment plans, and responses to interventions, thereby enhancing continuity of care and supporting clinical decision-making. Furthermore, this form is crucial for maintaining compliance with legal and regulatory standards, ensuring that all necessary information is documented accurately and comprehensively.
Dos and Don'ts
When filling out the Progress Notes form, it’s essential to follow certain guidelines to ensure accuracy and clarity. Here’s a list of things you should and shouldn’t do:
- Do write the date clearly at the top of the form.
- Do include the patient's full name, including last, first, and middle names.
- Do provide the patient's identification details, such as grade, rank, and rate.
- Do ensure the register number and ward number are filled out correctly.
- Do keep your notes concise and focused on relevant medical information.
- Don’t use abbreviations that may not be universally understood.
- Don’t leave any sections blank; fill out all required fields.
- Don’t include personal opinions or irrelevant details in the notes.
- Don’t forget to sign and date the form after completing it.
Document Attributes
| Fact Name | Description |
|---|---|
| Purpose | The Progress Notes form is used to document patient care and treatment in medical records. |
| Identification | It requires the patient's identification details, including name, grade, rank, and medical facility. |
| Standardization | This form is a standardized document known as Standard Form 509, revised in July 1991. |
| Governing Laws | The use of this form is governed by federal regulations outlined in 41 CFR 201-9.202-1. |
| Documentation | Progress notes should be clear and concise, providing an accurate record of the patient's condition and treatment. |
| Confidentiality | Patient information documented in this form must be kept confidential and secure, in compliance with HIPAA regulations. |
Key takeaways
When filling out and using the Progress Notes form, keep the following key takeaways in mind:
- Ensure you include the date of the entry at the top of the form.
- Provide the patient’s full name, including last, first, and middle names, as well as their grade, rank, and rate.
- Document the hospital or medical facility where the patient is receiving care.
- Utilize the standard format of the form to maintain consistency and clarity.
- Make sure to include the register number and ward number for accurate identification.
- Progress notes should be clear and concise, focusing on relevant medical information.
- Review and update the notes regularly to reflect the patient’s current condition and treatment.
- Keep the notes confidential and secure, as they are part of the patient’s medical record.
- Use the reverse side of the form if additional space is needed for detailed entries.
Other PDF Templates
Megger Test Sheet - The formal document creates a comprehensive record for future evaluations.
A Texas Last Will and Testament form is a legal document that outlines how an individual's assets and affairs should be managed after their death. This form allows individuals to express their wishes regarding the distribution of their property and the care of any dependents. Understanding its importance can help ensure that one's intentions are honored and that loved ones are taken care of. For those looking to create this important document, templates are available, such as the one provided by Texas Forms Online.
How Do I Get a P45 - The leaving date must be accurately filled out so that tax matters are addressed correctly.
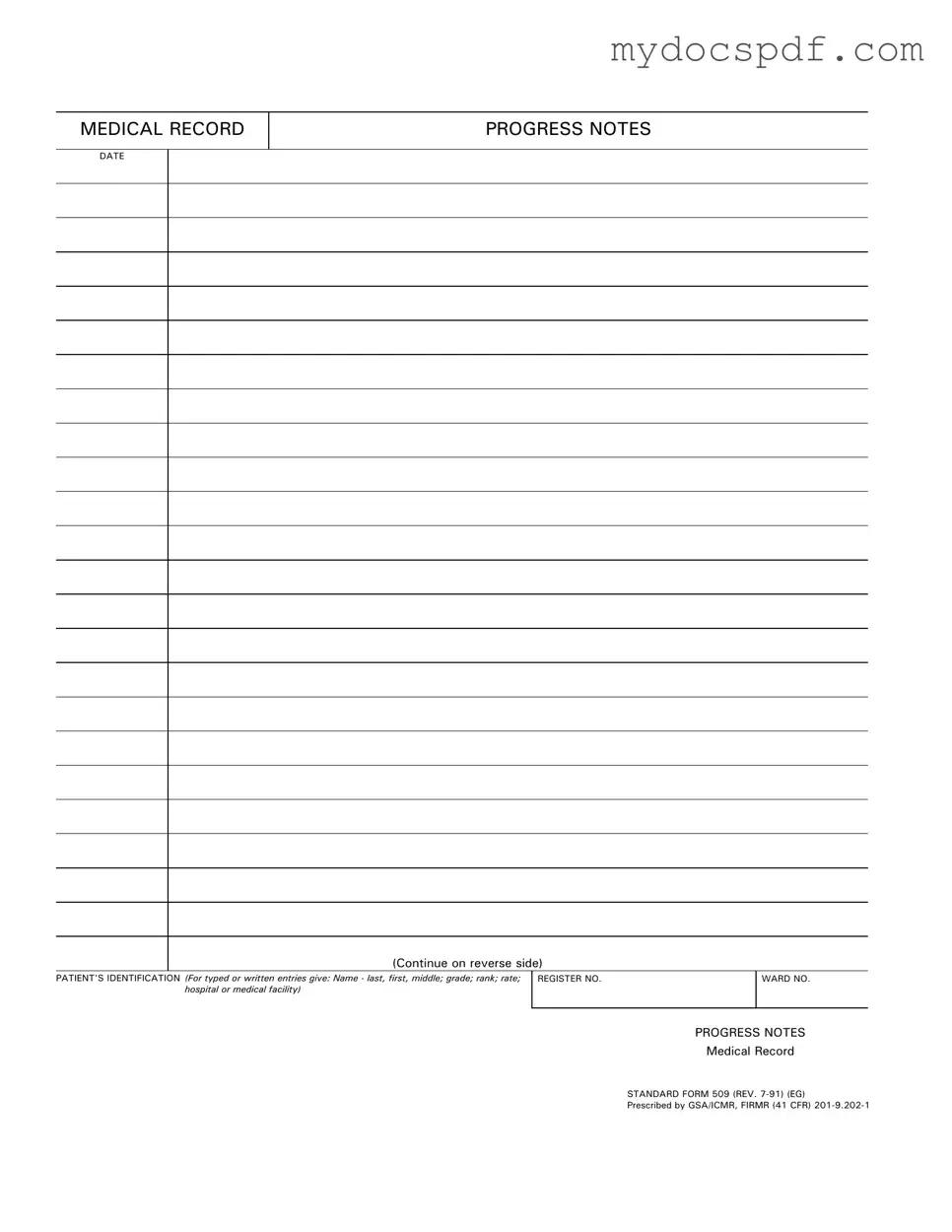
Example - Progress Notes Form
MEDICAL RECORD
PROGRESS NOTES
DATE
(Continue on reverse side)
PATIENT'S IDENTIFICATION (For typed or written entries give: Name - last, first, middle; grade; rank; rate; hospital or medical facility)
REGISTER NO. |
WARD NO. |
|
|
PROGRESS NOTES
Medical Record
STANDARD FORM 509 (REV.
Prescribed by GSA/ICMR, FIRMR (41 CFR)
PROGRESS NOTES
DATE
STANDARD FORM 509 (REV.
Detailed Instructions for Writing Progress Notes
Once you have the Progress Notes form in front of you, it’s important to ensure that all required fields are filled out accurately. This will help maintain clear and effective communication regarding the patient's medical record. Follow these steps carefully to complete the form.
- Locate the DATE section at the top of the form and enter the current date.
- In the PATIENT'S IDENTIFICATION section, provide the patient's full name, including last name, first name, and middle name.
- Next, include the patient's grade, rank, and rate as applicable.
- Identify the hospital or medical facility where the patient is receiving care.
- Fill in the REGISTER NO. which is usually assigned to the patient for record-keeping purposes.
- Then, enter the WARD NO. where the patient is located, if applicable.
- In the PROGRESS NOTES section, write detailed notes about the patient's condition, treatment, and any other relevant information.
After completing these steps, review the form to ensure all information is accurate and legible. This attention to detail will support effective patient care and documentation practices.
Documents used along the form
The Progress Notes form is an essential document in medical records, capturing vital information about a patient's treatment and progress. Alongside this form, several other documents are commonly utilized to ensure comprehensive patient care and accurate record-keeping. Below is a list of these documents, each serving a unique purpose in the healthcare process.
- Patient Intake Form: This document collects initial information about the patient, including personal details, medical history, and current medications. It helps healthcare providers understand the patient's background and tailor their care accordingly.
- Treatment Plan: A treatment plan outlines the specific interventions and goals for a patient’s care. It is developed collaboratively by the healthcare team and the patient, ensuring that everyone is aligned on the course of action.
- Consent Form: This form is crucial for obtaining a patient's permission before proceeding with treatment or procedures. It ensures that patients are informed about the risks and benefits, promoting transparency and trust in the patient-provider relationship.
- Boat Bill of Sale Form: For a successful transfer of boat ownership, be sure to utilize the detailed Boat Bill of Sale form guide to ensure compliance with legal standards.
- Discharge Summary: After a patient is discharged from care, a discharge summary provides a concise overview of their treatment, progress, and follow-up instructions. This document is vital for continuity of care, especially if the patient transitions to another provider.
- Referral Form: When a healthcare provider needs to refer a patient to a specialist, a referral form is used. This document includes pertinent information about the patient's condition and the reason for the referral, facilitating effective communication between providers.
- Medication Administration Record (MAR): The MAR tracks all medications administered to a patient during their stay. It ensures that dosages are accurately recorded and helps prevent medication errors, thereby enhancing patient safety.
These documents work together to create a comprehensive and cohesive medical record. Each plays a critical role in ensuring that patients receive safe, effective, and well-coordinated care throughout their treatment journey.