Get Annual Physical Examination Form in PDF
The Annual Physical Examination form is a crucial document that plays a significant role in maintaining your health and well-being. Completing this form accurately is essential to ensure a smooth and efficient medical appointment. It requires personal details, including your name, date of birth, and contact information, which help healthcare providers understand your background. Additionally, it prompts you to disclose any significant health conditions, current medications, and allergies, allowing for a comprehensive overview of your medical history. Immunization records are also a vital part of the form, as they help track your vaccinations and ensure you are up-to-date on necessary shots. The form includes sections for various medical tests, from tuberculosis screenings to prostate exams, tailored to specific age groups and genders. Furthermore, it addresses general physical examination details, such as blood pressure and weight, along with a thorough evaluation of different body systems. By gathering this information, the form assists healthcare professionals in making informed decisions regarding your health and any necessary follow-up care. Completing the Annual Physical Examination form not only facilitates better healthcare but also empowers you to take an active role in your health management.
Dos and Don'ts
Do's:
- Fill out all sections completely to avoid delays.
- Use clear and legible handwriting if completing the form by hand.
- Double-check your personal information for accuracy.
- List all current medications, including dosages and frequencies.
Don'ts:
- Do not leave any required fields blank.
- Avoid using abbreviations that may confuse the healthcare provider.
- Do not forget to include any allergies or sensitivities.
- Refrain from providing outdated medical history or incorrect information.
Document Attributes
| Fact Name | Fact Description |
|---|---|
| Purpose | The Annual Physical Examination form is designed to collect comprehensive health information prior to a medical appointment. |
| Completion Requirement | Patients must complete all sections of the form to minimize the need for return visits. |
| Health History | Patients are asked to provide a summary of their medical history, including chronic health problems and current medications. |
| Immunizations | The form includes a section for documenting immunizations, such as Tetanus, Hepatitis B, and Influenza. |
| Screening Tests | Various screening tests are listed, including TB screening, GYN exams, mammograms, and prostate exams, with specified frequencies. |
| Legal Compliance | In some states, the form must comply with specific healthcare regulations, such as the Health Insurance Portability and Accountability Act (HIPAA). |
| Physician's Role | The form requires the physician's signature, affirming that the examination has been conducted and reviewed. |
| Patient Information | It collects essential patient information, including name, date of birth, and contact details, to ensure accurate medical records. |
Key takeaways
Filling out and using the Annual Physical Examination form is a critical step in maintaining one’s health. Here are five key takeaways to ensure effective completion and use of the form:
- Complete All Sections: Every section of the form must be filled out thoroughly. Incomplete forms can lead to delays and additional visits, which can be inconvenient for both patients and healthcare providers.
- Provide Accurate Medical History: Include a detailed medical history, chronic health problems, and current medications. This information is vital for the physician to make informed decisions about your care.
- List Allergies and Sensitivities: Clearly indicate any allergies or sensitivities to medications. This information is crucial to avoid adverse reactions during treatment.
- Document Immunizations: Ensure that all immunization dates are accurately recorded. Keeping track of vaccinations helps in assessing overall health and compliance with preventive care guidelines.
- Review Recommendations: After the examination, carefully review any recommendations made by the physician. This includes follow-up tests, lifestyle changes, or referrals to specialists, which are essential for ongoing health management.
Other PDF Templates
Letter of Intent to Purchase - It is important for both parties to understand the letter's limited binding nature.
The Texas Affidavit of Correction form serves as a legal document that allows individuals to correct mistakes in public records. This form is essential for ensuring that inaccuracies, such as typographical errors or incorrect information, are amended properly. For those looking to obtain a template for this process, Texas Forms Online offers a convenient solution. By submitting this affidavit, individuals can maintain the integrity of their official documents and public records.
Car Repair Estimate Template - Estimate car repair costs and plan your budget effectively.
Example - Annual Physical Examination Form
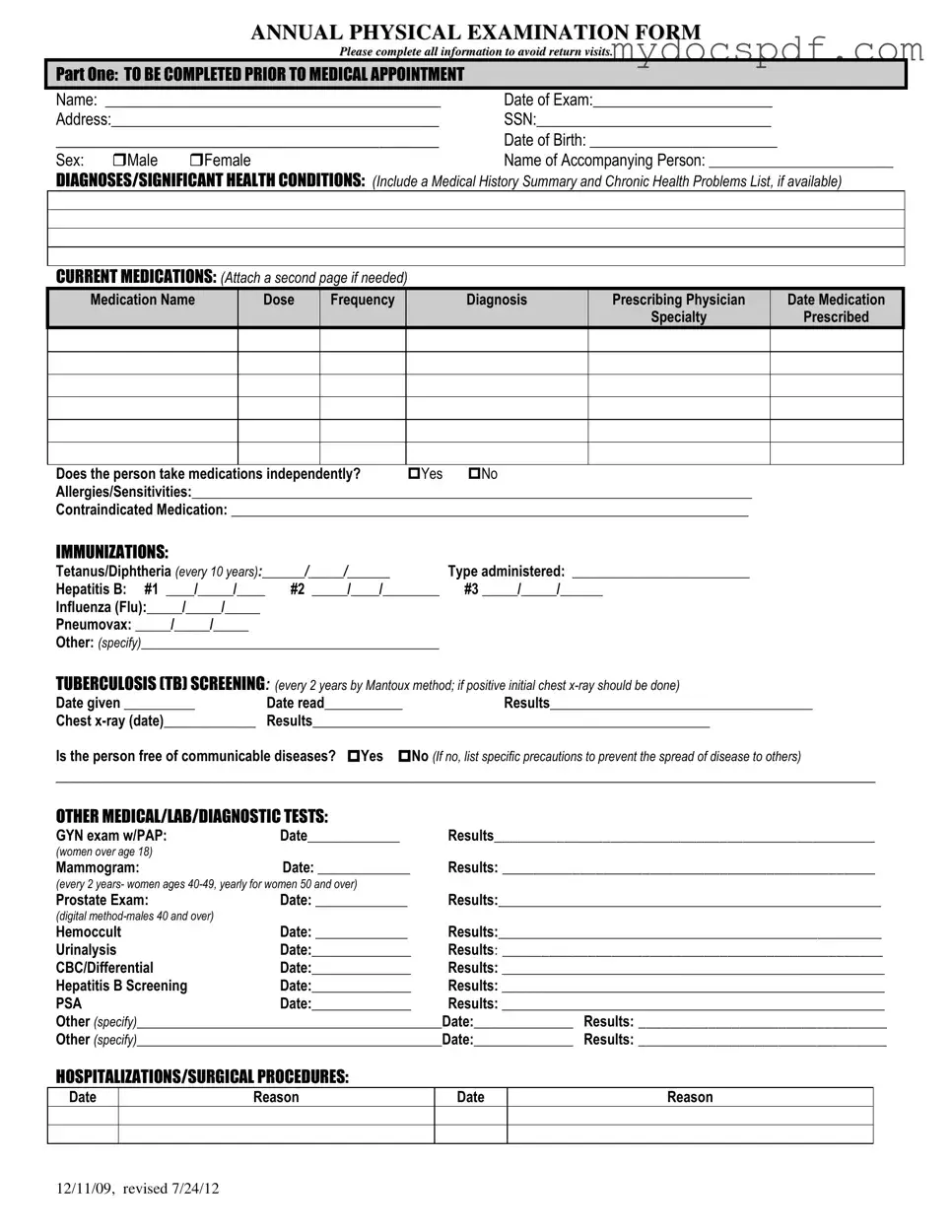
ANNUAL PHYSICAL EXAMINATION FORM
Please complete all information to avoid return visits.
PART ONE: TO BE COMPLETED PRIOR TO MEDICAL APPOINTMENT
Name: ___________________________________________ |
Date of Exam:_______________________ |
Address:__________________________________________ |
SSN:______________________________ |
_____________________________________________ |
Date of Birth: ________________________ |
||
Sex: |
Male |
Female |
Name of Accompanying Person: __________________________ |
DIAGNOSES/SIGNIFICANT HEALTH CONDITIONS: (Include a Medical History Summary and Chronic Health Problems List, if available)
CURRENT MEDICATIONS: (Attach a second page if needed)
Medication Name |
Dose |
Frequency |
Diagnosis |
Prescribing Physician |
Date Medication |
|
|
|
|
Specialty |
Prescribed |
Does the person take medications independently? |
Yes |
No |
Allergies/Sensitivities:_______________________________________________________________________________ |
||
Contraindicated Medication: _________________________________________________________________________
IMMUNIZATIONS:
Tetanus/Diphtheria (every 10 years):______/_____/______ |
Type administered: _________________________ |
|
Hepatitis B: #1 ____/_____/____ |
#2 _____/____/________ |
#3 _____/_____/______ |
Influenza (Flu):_____/_____/_____ |
|
|
Pneumovax: _____/_____/_____ |
|
|
Other: (specify)__________________________________________ |
|
|
TUBERCULOSIS (TB) SCREENING: (every 2 years by Mantoux method; if positive initial chest |
||
Date given __________ |
Date read___________ |
Results_____________________________________ |
Chest |
Results________________________________________________________ |
|
Is the person free of communicable diseases? Yes No (If no, list specific precautions to prevent the spread of disease to others)
_________________________________________________________________________________________________________
OTHER MEDICAL/LAB/DIAGNOSTIC TESTS:
GYN exam w/PAP: |
Date_____________ |
Results_________________________________________________ |
(women over age 18) |
|
|
Mammogram: |
Date: _____________ |
Results: ________________________________________________ |
(every 2 years- women ages
Prostate Exam: |
Date: _____________ |
Results:______________________________________________________ |
|
(digital |
|
|
|
Hemoccult |
Date: _____________ |
Results:______________________________________________________ |
|
Urinalysis |
Date:______________ |
Results: _________________________________________________ |
|
CBC/Differential |
Date:______________ |
Results: ______________________________________________________ |
|
Hepatitis B Screening |
Date:______________ |
Results: ______________________________________________________ |
|
PSA |
Date:______________ |
Results: ______________________________________________________ |
|
Other (specify)___________________________________________Date:______________ |
Results: ________________________________ |
||
Other (specify)___________________________________________Date:______________ |
Results: ________________________________ |
||
HOSPITALIZATIONS/SURGICAL PROCEDURES:
Date
Reason
Date
Reason
12/11/09, revised 7/24/12

PART TWO: GENERAL PHYSICAL EXAMINATION
|
|
|
|
|
Please complete all information to avoid return visits. |
|
|
|
|
|
Blood Pressure:______ /_______ Pulse:_________ |
Respirations:_________ Temp:_________ Height:_________ |
Weight:_________ |
||||
|
|
EVALUATION OF SYSTEMS |
|
|
|
|
||
|
|
|
|
|
|
|
||
|
|
System Name |
|
Normal Findings? |
Comments/Description |
|
||
|
|
Eyes |
|
Yes |
No |
|
|
|
|
|
Ears |
|
Yes |
No |
|
|
|
|
|
Nose |
|
Yes |
No |
|
|
|
|
|
Mouth/Throat |
|
Yes |
No |
|
|
|
|
|
Head/Face/Neck |
|
Yes |
No |
|
|
|
|
|
Breasts |
|
Yes |
No |
|
|
|
|
|
Lungs |
|
Yes |
No |
|
|
|
|
|
Cardiovascular |
|
Yes |
No |
|
|
|
|
|
Extremities |
|
Yes |
No |
|
|
|
|
|
Abdomen |
|
Yes |
No |
|
|
|
|
|
Gastrointestinal |
|
Yes |
No |
|
|
|
|
|
Musculoskeletal |
|
Yes |
No |
|
|
|
|
|
Integumentary |
|
Yes |
No |
|
|
|
|
|
Renal/Urinary |
|
Yes |
No |
|
|
|
|
|
Reproductive |
|
Yes |
No |
|
|
|
|
|
Lymphatic |
|
Yes |
No |
|
|
|
|
|
Endocrine |
|
Yes |
No |
|
|
|
|
|
Nervous System |
|
Yes |
No |
|
|
|
|
|
VISION SCREENING |
|
Yes |
No |
Is further evaluation recommended by specialist? |
Yes |
No |
|
|
HEARING SCREENING |
|
Yes |
No |
Is further evaluation recommended by specialist? |
Yes |
No |
|
|
ADDITIONAL COMMENTS: |
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
Medical history summary reviewed? |
Yes |
No |
|
|
||
Medication added, changed, or deleted: (from this appointment)__________________________________________________________
Special medication considerations or side effects: ________________________________________________________________
Recommendations for health maintenance: (include need for lab work at regular intervals, treatments, therapies, exercise, hygiene, weight control, etc.)
___________________________________________________________________________________________________________
Recommendations for manual breast exam or manual testicular exam: (include who will perform and frequency)____________________
___________________________________________________________________________________________________________
Recommended diet and special instructions: ____________________________________________________________________
Information pertinent to diagnosis and treatment in case of emergency:
___________________________________________________________________________________________________________
Limitations or restrictions for activities (including work day, lifting, standing, and bending): No Yes (specify)
___________________________________________________________________________________________________________ |
|||
Does this person use adaptive equipment? |
No |
Yes (specify):________________________________________________ |
|
Change in health status from previous year? No |
Yes (specify):_________________________________________________ |
||
This individual is recommended for ICF/ID level of care? (see attached explanation) Yes |
No |
||
Specialty consults recommended? No |
Yes (specify):_________________________________________________________ |
||
Seizure Disorder present? No Yes (specify type):__________________________________ Date of Last Seizure: ______________ |
|||
________________________________ |
_______________________________ |
_________________ |
|
Name of Physician (please print) |
Physician’s Signature |
|
Date |
Physician Address: _____________________________________________ |
Physician Phone Number: ____________________________ |
||
12/11/09, revised 7/24/12
Detailed Instructions for Writing Annual Physical Examination
Completing the Annual Physical Examination form is an important step to ensure that your healthcare provider has all the necessary information about your health. This helps avoid any delays in your appointment and ensures that your medical history is accurately recorded. Follow these steps to fill out the form correctly.
- Start with **Part One**. Fill in your Name at the top of the form.
- Next, write the Date of Exam.
- Provide your Address and Social Security Number (SSN).
- Enter your Date of Birth and select your Sex by checking the appropriate box.
- Write the name of the Accompanying Person, if applicable.
- List any Diagnoses/Significant Health Conditions. Include a summary of your medical history and any chronic health problems.
- Under Current Medications, fill in the details for each medication, including the name, dose, frequency, diagnosis, prescribing physician, and date prescribed. Attach a second page if necessary.
- Indicate whether you take medications independently by checking 'Yes' or 'No'.
- List any Allergies/Sensitivities you may have.
- Note any Contraindicated Medication.
- For Immunizations, fill in the dates for each vaccine you have received.
- Complete the Tuberculosis (TB) Screening section by providing the date given, date read, and results.
- Fill in the details for any Other Medical/Lab/Diagnostic Tests you have had, including dates and results.
- Document any Hospitalizations/Surgical Procedures with dates and reasons.
- Move to **Part Two**. Start by entering your Blood Pressure, Pulse, Respirations, Temperature, Height, and Weight.
- For the Evaluation of Systems, indicate whether each system has normal findings by checking 'Yes' or 'No'.
- Complete the Vision Screening and Hearing Screening sections, noting if further evaluation is recommended.
- Provide any Additional Comments that may be relevant to your health.
- Indicate whether your medical history summary has been reviewed.
- Document any changes to your medications during this appointment.
- List any recommendations for health maintenance, including lab work and exercise.
- Note any recommendations for manual breast or testicular exams.
- Provide details on recommended diet and special instructions.
- Include any information pertinent to diagnosis and treatment in case of an emergency.
- Specify any limitations or restrictions for activities.
- Indicate whether you use adaptive equipment.
- Note any changes in health status from the previous year.
- Answer whether the individual is recommended for ICF/ID level of care.
- List any specialty consults recommended.
- Indicate if a seizure disorder is present and provide the date of the last seizure.
- Finally, fill in the physician's name, signature, date, address, and phone number at the bottom of the form.
Once you have completed the form, review it for accuracy and completeness. Make sure all sections are filled out to avoid any need for follow-up visits. Bring the form with you to your appointment to ensure a smooth and efficient process.
Documents used along the form
The Annual Physical Examination form is an essential document that helps healthcare providers assess a patient's overall health. However, several other forms and documents often accompany it to ensure comprehensive care. Each of these documents serves a specific purpose in the medical evaluation process.
- Medical History Form: This document collects detailed information about a patient's past medical conditions, surgeries, and family health history. It helps physicians understand the patient's background and any potential health risks.
- Immunization Record: This record lists all vaccinations a patient has received, including dates and types. It is crucial for tracking immunizations and ensuring patients are up-to-date with required vaccines.
- Consent for Treatment Form: Patients sign this form to give healthcare providers permission to perform examinations and treatments. It ensures that patients are informed about the procedures they will undergo and agree to them voluntarily.
- Lab Test Requisition: This document is used to order specific laboratory tests based on the findings from the physical examination. It includes details about the tests needed and any relevant patient information to guide the lab in processing samples accurately.
- Residential Lease Agreement: The NY Templates offers a framework that ensures both landlords and tenants are clear on their rights and responsibilities, contributing to a respectful and harmonious living arrangement.
- Referral Form: If a patient requires specialized care, a referral form is used to direct them to another healthcare provider. This form typically includes the reason for the referral and any pertinent medical information to assist the specialist in providing care.
These accompanying documents play a vital role in ensuring that the healthcare process is thorough and effective. Together with the Annual Physical Examination form, they help create a complete picture of a patient’s health and facilitate better medical decision-making.